Mucoepidermoid carcinoma
| Mucoepidermoid carcinoma | |
|---|---|
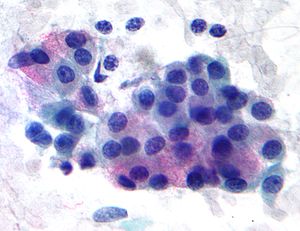 | |
| Micrograph of a mucoepidermoid carcinoma. FNA specimen. Pap stain. | |
| Specialty | Oncology, Maxillofacial surgery, ENT surgery |
Mucoepidermoid carcinoma (MEC)[1] is the most common type of minor salivary gland malignancy in adults. Mucoepidermoid carcinoma can also be found in other organs, such as bronchi, lacrimal sac,[2] and thyroid gland.
Mucicarmine staining is one stain used by pathologist for detection.[3]
Signs and symptoms[edit]
Presents as painless, slow-growing mass that is firm or hard. Most appear clinically as mixed tumors. Usually occurs at 30–50 years of age. More predilection towards female sex.[citation needed]
Diagnosis[edit]
Histology[edit]
This tumor is not encapsulated and is characterized by squamous cells, mucus-secreting cells, and intermediate cells.[4]
Molecular biology[edit]
Mucoepidermoid carcinomas of the salivary and bronchial glands are characterized by a recurrent t(11;19)(q21;p13) chromosomal translocation resulting in a MECT1-MAML2 fusion gene.[5] The CREB-binding domain of the CREB coactivator MECT1 (also known as CRTC1, TORC1 or WAMTP1) is fused to the transactivation domain of the Notch coactivator MAML2.[6]
A possible association with papillomavirus has been reported.[7]
Prognosis[edit]
Generally, there is a good prognosis for low-grade tumors, and a poor prognosis for high-grade tumors, however recent research have found reoccurring low grade tumors also have a poor prognosis.[8]
Treatment[edit]
Surgery is the recommended treatment for localised resectable disease.[9] When the tumour is incompletely resected (positive margins) post-operative radiotherapy gives local control comparable to a complete resection (clear margins).[10]
Sometimes when surgery is not possible due to extent of disease or if a patient is too frail for surgery, or declines surgery, palliative radiotherapy may be helpful. There has been a report of a case where low dose radiotherapy achieve disease response and control for more than 4 years.[11]
In patients with metastatic disease, chemotherapy response tends to be low (27% partial response rate) and short lived.[12]
Epidemiology[edit]
Occurs in adults, with peak incidence from 20–40 years of age. A causal link with cytomegalovirus (CMV) has been strongly implicated in a 2011 research.[13]
Relative incidence of parotid tumors, showing mucoepidermoid carcinoma at top right.[14]
Relative incidence of submandibular tumors, showing mucoepidermoid carcinoma at top right.[14]
References[edit]
- ^ Kalhor N, Moran CA (March 2018). "Pulmonary mucoepidermoid carcinoma: diagnosis and treatment". Expert Review of Respiratory Medicine. 12 (3): 249–255. doi:10.1080/17476348.2018.1428563. PMID 29338644.
- ^ Williams JD, Agrawal A, Wakely PE (February 2003). "Mucoepidermoid carcinoma of the lacrimal sac". Annals of Diagnostic Pathology. 7 (1): 31–34. doi:10.1053/adpa.2003.50005. PMID 12616472.
- ^ Baloch ZW, Solomon AC, LiVolsi VA (July 2000). "Primary mucoepidermoid carcinoma and sclerosing mucoepidermoid carcinoma with eosinophilia of the thyroid gland: a report of nine cases". Modern Pathology. 13 (7): 802–807. doi:10.1038/modpathol.3880140. PMID 10912941.
- ^ Chenevert J, Barnes LE, Chiosea SI (February 2011). "Mucoepidermoid carcinoma: a five-decade journey". Virchows Archiv. 458 (2): 133–140. doi:10.1007/s00428-011-1040-y. PMID 21243374.
- ^ Chiosea SI, Dacic S, Nikiforova MN, Seethala RR (August 2012). "Prospective testing of mucoepidermoid carcinoma for the MAML2 translocation: clinical implications". The Laryngoscope. 122 (8): 1690–1694. doi:10.1002/lary.22419. PMID 22833306.
- ^ Behboudi A, Enlund F, Winnes M, Andrén Y, Nordkvist A, Leivo I, et al. (May 2006). "Molecular classification of mucoepidermoid carcinomas-prognostic significance of the MECT1-MAML2 fusion oncogene". Genes, Chromosomes & Cancer. 45 (5): 470–481. doi:10.1002/gcc.20306. PMID 16444749.
- ^ Isayeva T, Said-Al-Naief N, Ren Z, Li R, Gnepp D, Brandwein-Gensler M (June 2013). "Salivary mucoepidermoid carcinoma: demonstration of transcriptionally active human papillomavirus 16/18". Head and Neck Pathology. 7 (2): 135–148. doi:10.1007/s12105-012-0411-2. PMC 3642267. PMID 23233027.
- ^ Rubin A, Davis J, Jreije K, Wu H, Oppenheimer R (2017). "Case Report: Recurrent Mucoepidermoid Carcinoma of the Tongue in Adult Female Patient With Lung Cancer". Clinical Medicine Insights. Ear, Nose and Throat. 10: 1179550617720462. doi:10.1177/1179550617720462. PMC 5513522. PMID 28757800.
- ^ Verma J, Teh BS, Paulino AC (December 2011). "Characteristics and outcome of radiation and chemotherapy-related mucoepidermoid carcinoma of the salivary glands". Pediatric Blood & Cancer. 57 (7): 1137–1141. doi:10.1002/pbc.22978. PMID 21280198.
- ^ Hosokawa Y, Shirato H, Kagei K, Hashimoto S, Nishioka T, Tei K, et al. (January 1999). "Role of radiotherapy for mucoepidermoid carcinoma of salivary gland". Oral Oncology. 35 (1): 105–111. doi:10.1016/s1368-8375(98)00053-0. PMID 10211318.
- ^ Vulpe H, Giuliani M, Goldstein D, Perez-Ordonez B, Dawson LA, Hope A (October 2013). "Long term control of a maxillary sinus mucoepidermoid carcinoma with low dose radiation therapy: a case report". Radiation Oncology. 8: 251. doi:10.1186/1748-717X-8-251. PMC 3829377. PMID 24165756.
- ^ Licitra L, Cavina R, Grandi C, Palma SD, Guzzo M, Demicheli R, Molinari R (August 1996). "Cisplatin, doxorubicin and cyclophosphamide in advanced salivary gland carcinoma. A phase II trial of 22 patients". Annals of Oncology. 7 (6): 640–642. doi:10.1093/oxfordjournals.annonc.a010684. PMID 8879381.
- ^ Melnick M, Sedghizadeh PP, Allen CM, Jaskoll T (February 2012). "Human cytomegalovirus and mucoepidermoid carcinoma of salivary glands: cell-specific localization of active viral and oncogenic signaling proteins is confirmatory of a causal relationship". Experimental and Molecular Pathology. 92 (1): 118–125. doi:10.1016/j.yexmp.2011.10.011. PMID 22101257.
- ^ a b Steve C Lee, MD, PhD. "Salivary Gland Neoplasms". Medscape.
{{cite web}}: CS1 maint: multiple names: authors list (link) Updated: Jan 13, 2021}}
Diagrams by Mikael Häggström, MD




![Relative incidence of parotid tumors, showing mucoepidermoid carcinoma at top right.[14]](http://upload.wikimedia.org/wikipedia/commons/thumb/b/b1/Relative_incidence_of_parotid_tumors.png/477px-Relative_incidence_of_parotid_tumors.png)
![Relative incidence of submandibular tumors, showing mucoepidermoid carcinoma at top right.[14]](http://upload.wikimedia.org/wikipedia/commons/thumb/a/a7/Relative_incidence_of_submandibular_tumors.png/479px-Relative_incidence_of_submandibular_tumors.png)
No comments:
Post a Comment