Hereditary nonpolyposis colorectal cancer
| Hereditary nonpolyposis colorectal cancer | |
|---|---|
| Other names | Lynch syndrome[1] |
 | |
| Micrograph showing tumor-infiltrating lymphocytes (in a colorectal cancer), a finding associated with MSI-H tumours, as may be seen in Lynch syndrome. H&E stain. | |
| Specialty | Oncology |
Hereditary nonpolyposis colorectal cancer (HNPCC) or Lynch syndrome is an autosomal dominant genetic condition that is associated with a high risk of colon cancer[2] as well as other cancers including endometrial cancer (second most common), ovary, stomach, small intestine, hepatobiliary tract, upper urinary tract, brain, and skin. The increased risk for these cancers is due to inherited mutations that impair DNA mismatch repair. It is a type of cancer syndrome.
Contents
Signs and symptoms[edit]
Risk of cancer[edit]
Lifetime risk and mean age at diagnosis for Lynch syndrome associated cancers[3]
| Type of cancer | Lifetime risk (%) | Mean age at diagnosis (years) |
| Colorectal | 52-58 | 44-61 |
| Endometrial | 25-60 | 48-62 |
| Gastric | 6-13 | 56 |
| Ovarian | 4-12 | 42.5 |
In addition to the types of cancer found in the chart above, it is understood that Lynch syndrome also contributes to an increased risk of small bowel cancer, pancreatic cancer, ureter/renal pelvis cancer, biliary tract cancer, brain cancer, and sebaceous neoplasms.[3] Increased risk of prostate cancer and breast cancer has also been associated with Lynch syndrome, although this relationship is not entirely understood.[3]
Two-thirds of colon cancers occur in the proximal colon. The mean age of colorectal cancer diagnosis is 44 for members of families that meet the Amsterdam criteria. The average age of diagnosis of endometrial cancer is about 46 years. Among women with HNPCC who have both colon and endometrial cancer, about half present first with endometrial cancer, making endometrial cancer the most common sentinel cancer in Lynch syndrome.[4] In HNPCC, the mean age of diagnosis of gastric cancer is 56 years of age with intestinal-type adenocarcinoma being the most commonly reported pathology. HNPCC-associated ovarian cancers have an average age of diagnosis of 42.5 years-old; approximately 30% are diagnosed before age 40.
A large follow up study (3119 patients; average follow up 24 years) has found significant variation in the cancer rates depending on the mutation involved.[5] Up to the age of 75 years the risks of colorectal cancer, endometrial cancer, ovarian cancer, upper gastrointestinal (gastric, duodenal, bile duct or pancreatic), urinary tract cancers, prostate cancer and brain tumours were as follows: for MLH1 mutations the risk was - 46%, 43%, 10%, 21%, 8%, 17% and 1% respectively: for MSH2 mutations the risks were 57%, 17%, 10%, 25%, 32%, and 5% respectively: for MSH6 mutations the risks were 15%, 46%, 13%, 7%, 11%, 18% and 1% respectively.
| Gene | Ovarian cancer risk | Endometrial cancer risk |
|---|---|---|
| MLH1 | 4-24% | 25-60% |
| MSH2/EPCAM | 4-24% | 25-60% |
| MSH6 | 1-11% | 16-26% |
| PMS2 | 6% (combined risk) | 15% |
Genetics[edit]
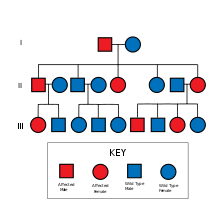
HNPCC is inherited in an autosomal dominant fashion.[7] The hallmark of HNPCC is defective DNA mismatch repair, which leads to microsatellite instability, also known as MSI-H (the H is "high"). MSI is identifiable in cancer specimens in the pathology laboratory.[8] Most cases result in changes in the lengths of dinucleotide repeats of the nucleobases cytosine and adenine (sequence: CACACACACA...).[9]
The 4 main genes involved in HNPCC normally encode for proteins that form dimers to function:
- MLH1 protein dimerizes with PMS2 protein to form MutLα, which coordinates the binding of other proteins involved with mismatch repair like DNA helicase, single-stranded-DNA binding-protein (RPA), and DNA polymerases.[10][11]
- MSH2 protein dimerizes with MSH6 protein, which identifies mismatches via a sliding clamp model, a protein for scanning for errors.[12][13]
The impairment of either gene for the protein dimer impairs the protein function.[14] These 4 genes are involved in error correction (mismatch repair), so dysfunction of the genes can lead to the inability to fix DNA replication errors and cause HNPCC.[15] HNPCC is known to be associated with other mutations in genes involved in the DNA mismatch repair pathway:
| OMIM name | Genes implicated in HNPCC | Frequency of mutations in HNPCC families | Locus | First publication |
|---|---|---|---|---|
| HNPCC1 (120435) | MSH2/EPCAM | approximately 60% | 2p22 | Fishel 1993[16] |
| HNPCC2 (609310) | MLH1 | approximately 30% | 3p21 | Papadopoulos 1994[17] |
| HNPCC5 | MSH6 | 7-10% | 2p16 | Miyaki 1997[18] |
| HNPCC4 | PMS2 | relatively infrequent | 7p22[19] | Nicolaides 1994 |
| HNPCC3 | PMS1 | case report[19] | 2q31-q33 | Nicolaides 1994 |
| HNPCC6 | TGFBR2 | case report[20] | 3p22 | |
| HNPCC7 | MLH3 | disputed[21] | 14q24.3 |
People with MSH6 mutations are more likely to be Amsterdam criteria II-negative.[22] The presentation with MSH6 is slightly different than with MLH1 and MSH2, and the term "MSH6 syndrome" has been used to describe this condition.[23] In one study, the Bethesda guidelines were more sensitive than the Amsterdam Criteria in detecting it.[24]
Up to 39% of families with mutations in an HNPCC gene do not meet the Amsterdam criteria.[citation needed] Therefore, families found to have a deleterious mutation in an HNPCC gene should be considered to have HNPCC regardless of the extent of the family history. This also means that the Amsterdam criteria fail to identify many people who are at risk for Lynch syndrome. Improving the criteria for screening is an active area of research, as detailed in the Screening Strategies section of this article.
Most people with HNPCC inherit the condition from a parent. However, due to incomplete penetrance, variable age of cancer diagnosis, cancer risk reduction, or early death, not all people with an HNPCC gene mutation have a parent who had cancer. Some people develop HNPCC de-novo in a new generation, without inheriting the gene. These people are often only identified after developing an early-life colon cancer. Parents with HNPCC have a 50% chance of passing the genetic mutation on to each child. It is also important to note, that deleterious mutation in one of MMR genes alone is not sufficient to cause cancer, but that rather further mutations in other tumour suppressor genes need to occur.[25]
Diagnosis[edit]
A diagnosis of Lynch Syndrome is applied to people with a germline DNA mutation in one of the MMR genes (MLH1, MSH2, MSH6, and PMS2) or the EPCAM gene, identified by genetic testing.[26] Candidates for germline genetic testing can be identified by clinical criteria such as the Amsterdam Clinical Criteria and Bethesda Guidelines, or through tumor analysis by immunohistochemistry(IHC), or microsatellite instability (MSI) testing.[26] Genetic testing is commercially available and consists of a blood test.[citation needed]
Immunohistochemistry[edit]
Immunohistochemistry (IHC) is a method that can be used to detect abnormal mismatch repair (MMR) protein expression in tumours that are associated with Lynch syndrome. While it is not diagnostic of a Lynch syndrome, it can play a role in identifying people who should have germline testing.[27] Two methods of implementation of IHC testing includes age-based testing and universal testing for all people.[28] Currently, there is no widespread agreement regarding which screening method should be used.[28] Age-based testing for IHC has been suggested in part due to cost-benefit analyses, whereas universal testing for all people with colorectal cancer ensures people with Lynch Syndrome are not missed.[28]
Microsatellite Instability[edit]
Mutations in DNA mismatch repair systems can lead to difficulty transmitting regions within the DNA which contain repeating patterns of two or three nucleotides (microsatellites), otherwise known as microsatellite instability (MSI).[29] MSI is identified through DNA extraction from both a tumor tissue sample and a normal tissue sample followed by PCR analysis of microsatellite regions.[29] MSI analysis can be used to identify people who may have Lynch syndrome and direct them for further testing.[29]
Classification[edit]
Three major groups of MSI-H (microsatellite instability – MSI) cancers can be recognized by histopathological criteria:
- right-sided poorly differentiated cancers
- right-sided mucinous cancers
- adenocarcinomas in any location showing any measurable level of intraepithelial lymphocyte (TIL)
In addition, HNPCC can be divided into Lynch syndrome I (familial colon cancer) and Lynch syndrome II (HNPCC associated with other cancers of the gastrointestinal tract or reproductive system).[30]
Prevention[edit]
After reporting a null finding from their randomized controlled trial of aspirin (acetylsalicylic acid – ASA) to prevent the colorectal neoplasia of Lynch syndrome,[31] Burn and colleagues have reported new data, representing a longer follow-up period than reported in the initial NEJM paper. These new data demonstrate a reduced incidence in people with Lynch syndrome who were exposed to at least four years of high-dose aspirin, with a satisfactory risk profile.[32] These results have been widely covered in the media; future studies will look at modifying (lowering) the dose (to reduce risk associated with the high dosage of ASA).
Screening[edit]
Genetic counseling and genetic testing are recommended for families that meet the Amsterdam criteria, preferably before the onset of colon cancer.
A transvaginal ultrasound with or without endometrial biopsy is recommended annually for ovarian and endometrial cancer screening.[6]
Amsterdam criteria[edit]
The following are the Amsterdam criteria in identifying high-risk candidates for molecular genetic testing:[33]
Amsterdam I Criteria (all bullet points must be fulfilled): The Amsterdam I criteria were published in 1990; however, were felt to be insufficiently sensitive.[34]
- Three or more family members with a confirmed diagnosis of colorectal cancer, one of whom is a first degree (parent, child, sibling) relative of the other two
- Two successive affected generations
- One or more colon cancers diagnosed under age 50 years
- Familial adenomatous polyposis (FAP) has been excluded
The Amsterdam II criteria were developed in 1999 and improved the diagnostic sensitivity for Lynch Syndrome by including cancers of the endometrium, small bowel, ureter and renal pelvis.[35]
Amsterdam Criteria II (all bullet points must be fulfilled):[35]
- Three or more family members with HNPCC-related cancers, one of whom is a first-degree relative of the other two
- Two successive affected generations
- One or more of the HNPCC-related cancers diagnosed under age 50 years
- Familial adenomatous polyposis (FAP) has been excluded
The Bethesda criteria were developed in 1997 and later updated in 2004 by the National Cancer Institute to identify persons requiring further testing for Lynch Syndrome through MSI. In contrast to the Amsterdam Criteria, the Revised Bethesda Guidelines use pathological data in addition to clinical information to help health care providers identify persons at high-risk.[34][35]
Revised Bethesda Guidelines:
If a person meets any 1 of 5 criteria the tumour(s) from the person should be tested for MSI:[34]
1. Colorectal cancer diagnosed before age 50
2. Presence of synchronous or metachronous colorectal or other Lynch syndrome associated cancers (e.g. cancers of endometrium, ovary, stomach, small bowel, pancreas, biliary tract, ureter, renal pelvis, brain, sebaceous glands, keratoacanthomas)
3. Colorectal cancer with MSI-high pathology in a person who is younger than 60 years of age
4. Colorectal cancer diagnosed in a person with one or more first-degree relative with colorectal cancer or Lynch syndrome associated tumour diagnosed under age 50
5. Person with colorectal cancer and two or more first- or second-degree relatives with colorectal cancer or Lynch syndrome associated cancer diagnosed at any age[34][35]
It is important to note that these clinical criteria can be difficult to use in practice and clinical criteria used alone misses between 12 and 68 percent of Lynch Syndrome cases.[34]
Surgery[edit]
Prophylactic hysterectomy and salpingo-oophorectomy (removal of the uterus, Fallopian tubes, and ovaries to prevent cancer from developing) can be performed before ovarian or endometrial cancer develops.[6]
Treatment[edit]
Surgery remains the front-line therapy for HNPCC. There is an ongoing controversy over the benefit of 5-fluorouracil-based adjuvant therapies for HNPCC-related colorectal tumours, particularly those in stages I and II.[36]
- Anti-PD-1 antibody therapy can be effective.[37]
Epidemiology[edit]
In the United States, about 160,000 new cases of colorectal cancer are diagnosed each year. Hereditary nonpolyposis colorectal cancer is responsible for approximately 2 percent to 7 percent of all diagnosed cases of colorectal cancer. The average age of diagnosis of cancer in patients with this syndrome is 44 years old, as compared to 64 years old in people without the syndrome.[38]
Terminology[edit]
Henry T. Lynch, Professor of Medicine at Creighton University Medical Center, characterized the syndrome in 1966.[39] In his earlier work, he described the disease entity as "cancer family syndrome." The term "Lynch syndrome" was coined in 1984 by other authors; Lynch named the condition HNPCC in 1985. Since then the two terms have been used interchangeably, until later advances in the understanding of the genetics of the disease led to the term HNPCC falling out of favor.[40]
Other sources reserve the term "Lynch syndrome" when there is a known DNA mismatch repair defect, and use the term "familial colorectal cancer type X" when the Amsterdam criteria are met but there is no known DNA mismatch repair defect.[41] The putative "type X" families appear to have a lower overall incidence of cancer and lower risk for non-colorectal cancers than families with documented DNA mismatch repair deficiency.[42] About 35% of people who meet Amsterdam criteria do not have a DNA-mismatch-repair gene mutation.[43]
Complicating matters is the presence of an alternative set of criteria, known as the "Bethesda Guidelines."[44][45][46]
Society[edit]
There are a number of non-profit organisations providing information and support, including Lynch Syndrome International, Lynch Syndrome UK[47] and Bowel Cancer UK.[48] In the US, National Lynch Syndrome Awareness Day is March 22.[49]
References[edit]
- ^ "Lynch syndrome | Genetic and Rare Diseases Information Center (GARD) – an NCATS Program". rarediseases.info.nih.gov. Retrieved 4 October 2019.
- ^ Kastrinos F, Mukherjee B, Tayob N, Wang F, Sparr J, Raymond VM, et al. (October 2009). "Risk of pancreatic cancer in families with Lynch syndrome". JAMA. 302 (16): 1790–5. doi:10.1001/jama.2009.1529. PMC 4091624. PMID 19861671.
- ^ a b c "Lynch Syndrome". DynaMed. February 22, 2019. Retrieved November 18, 2019.
- ^ Hoffman BL (2012). "Chapter 33: Endometrial Cancer". Williams Gynecology (2nd ed.). New York: McGraw-Hill Medical. ISBN 978-0071716727.
- ^ Møller P, Seppälä TT, Bernstein I, Holinski-Feder E, Sala P, Gareth Evans D, et al. (July 2018). "path_MMR carriers by gene and gender up to 75 years of age: a report from the Prospective Lynch Syndrome Database". Gut. 67 (7): 1306–1316. doi:10.1136/gutjnl-2017-314057. PMC 6031262. PMID 28754778.
- ^ a b c Ring KL, Garcia C, Thomas MH, Modesitt SC (November 2017). "Current and future role of genetic screening in gynecologic malignancies". American Journal of Obstetrics and Gynecology. 217 (5): 512–521. doi:10.1016/j.ajog.2017.04.011. PMID 28411145.
- ^ "Lynch Syndrome". Genetics Home Reference.
- ^ Pathology of Hereditary Nonpolyposis Colorectal Cancer - JASS 910 (1): 62 - Annals of the New York Academy of Sciences Archived 2006-06-19 at the Wayback Machine
- ^ Oki E, Oda S, Maehara Y, Sugimachi K (March 1999). "Mutated gene-specific phenotypes of dinucleotide repeat instability in human colorectal carcinoma cell lines deficient in DNA mismatch repair". Oncogene. 18 (12): 2143–7. doi:10.1038/sj.onc.1202583. PMID 10321739.
- ^ Yokoyama, Takanori; Takehara, Kazuhiro; Sugimoto, Nao; Kaneko, Keika; Fujimoto, Etsuko; Okazawa-Sakai, Mika; Okame, Shinichi; Shiroyama, Yuko; Yokoyama, Takashi; Teramoto, Norihiro; Ohsumi, Shozo (December 2018). "Lynch syndrome-associated endometrial carcinoma with MLH1 germline mutation and MLH1 promoter hypermethylation: a case report and literature review". BMC Cancer. 18 (1): 576. doi:10.1186/s12885-018-4489-0. ISSN 1471-2407. PMC 5963021. PMID 29783979.
- ^ Peltomäki, Päivi (2003-03-15). "Role of DNA mismatch repair defects in the pathogenesis of human cancer". Journal of Clinical Oncology. 21 (6): 1174–1179. doi:10.1200/JCO.2003.04.060. ISSN 0732-183X. PMID 12637487.
- ^ Tamura, Kazuo; Kaneda, Motohide; Futagawa, Mashu; Takeshita, Miho; Kim, Sanghyuk; Nakama, Mina; Kawashita, Norihito; Tatsumi-Miyajima, Junko (September 2019). "Genetic and genomic basis of the mismatch repair system involved in Lynch syndrome". International Journal of Clinical Oncology. 24 (9): 999–1011. doi:10.1007/s10147-019-01494-y. ISSN 1341-9625.
- ^ Fishel, R.; Lescoe, M. K.; Rao, M. R.; Copeland, N. G.; Jenkins, N. A.; Garber, J.; Kane, M.; Kolodner, R. (1993-12-03). "The human mutator gene homolog MSH2 and its association with hereditary nonpolyposis colon cancer". Cell. 75 (5): 1027–1038. doi:10.1016/0092-8674(93)90546-3. ISSN 0092-8674. PMID 8252616.
- ^ Yurgelun, Matthew B.; Hampel, Heather (2018-05-23). "Recent Advances in Lynch Syndrome: Diagnosis, Treatment, and Cancer Prevention". American Society of Clinical Oncology Educational Book. American Society of Clinical Oncology. Annual Meeting. 38: 101–109. doi:10.1200/EDBK_208341. ISSN 1548-8756. PMID 30231390.
- ^ Le, Stephanie; Ansari, Umer; Mumtaz, Aisha; Malik, Kunal; Patel, Parth; Doyle, Amanda; Khachemoune, Amor (2017-11-15). "Lynch Syndrome and Muir-Torre Syndrome: An update and review on the genetics, epidemiology, and management of two related disorders". Dermatology Online Journal. 23 (11). ISSN 1087-2108. PMID 29447627.
- ^ Fishel R, Lescoe MK, Rao MR, Copeland NG, Jenkins NA, Garber J, et al. (December 1993). "The human mutator gene homolog MSH2 and its association with hereditary nonpolyposis colon cancer". Cell. 75 (5): 1027–38. doi:10.1016/0092-8674(93)90546-3. PMID 8252616.
- ^ Papadopoulos N, Nicolaides NC, Wei YF, Ruben SM, Carter KC, Rosen CA, et al. (March 1994). "Mutation of a mutL homolog in hereditary colon cancer". Science. 263 (5153): 1625–9. Bibcode:1994Sci...263.1625P. doi:10.1126/science.8128251. PMID 8128251.
- ^ Miyaki M, Konishi M, Tanaka K, Kikuchi-Yanoshita R, Muraoka M, Yasuno M, et al. (November 1997). "Germline mutation of MSH6 as the cause of hereditary nonpolyposis colorectal cancer". Nature Genetics. 17 (3): 271–2. doi:10.1038/ng1197-271. PMID 9354786.
- ^ a b Nicolaides NC, Papadopoulos N, Liu B, Wei YF, Carter KC, Ruben SM, et al. (September 1994). "Mutations of two PMS homologues in hereditary nonpolyposis colon cancer". Nature. 371 (6492): 75–80. Bibcode:1994Natur.371...75N. doi:10.1038/371075a0. PMID 8072530.
- ^ Lu SL, Kawabata M, Imamura T, Akiyama Y, Nomizu T, Miyazono K, Yuasa Y (May 1998). "HNPCC associated with germline mutation in the TGF-beta type II receptor gene". Nature Genetics. 19 (1): 17–8. doi:10.1038/ng0598-17. PMID 9590282.
- ^ Ou J, Rasmussen M, Westers H, Andersen SD, Jager PO, Kooi KA, et al. (April 2009). "Biochemical characterization of MLH3 missense mutations does not reveal an apparent role of MLH3 in Lynch syndrome" (PDF). Genes, Chromosomes & Cancer. 48 (4): 340–50. doi:10.1002/gcc.20644. PMID 19156873.
- ^ Ramsoekh D, Wagner A, van Leerdam ME, Dinjens WN, Steyerberg EW, Halley DJ, et al. (November 2008). "A high incidence of MSH6 mutations in Amsterdam criteria II-negative families tested in a diagnostic setting". Gut. 57 (11): 1539–44. doi:10.1136/gut.2008.156695. PMID 18625694.
- ^ Suchy J, Lubinski J (June 2008). "MSH6 syndrome". Hereditary Cancer in Clinical Practice. 6 (2): 103–4. doi:10.1186/1897-4287-6-2-103. PMC 2735474. PMID 19804606.
- ^ Goldberg Y, Porat RM, Kedar I, Shochat C, Galinsky D, Hamburger T, et al. (June 2010). "An Ashkenazi founder mutation in the MSH6 gene leading to HNPCC". Familial Cancer. 9 (2): 141–50. doi:10.1007/s10689-009-9298-9. PMID 19851887.
- ^ http://www.genetics.edu.au/publications-and-resources/facts-sheets/fact-sheet-33-bowel-cancer-and-inherited-predisposition
- ^ a b Giardiello, Francis M.; Allen, John I.; Axilbund, Jennifer E.; Boland, C. Richard; Burke, Carol A.; Burt, Randall W.; Church, James M.; Dominitz, Jason A.; Johnson, David A.; Kaltenbach, Tonya; Levin, Theodore R. (August 2014). "Guidelines on Genetic Evaluation and Management of Lynch Syndrome: A Consensus Statement by the US Multi-Society Task Force on Colorectal Cancer". Gastroenterology. 147 (2): 502–526. doi:10.1053/j.gastro.2014.04.001.
- ^ Snowsill, Tristan; Huxley, Nicola; Hoyle, Martin; Jones-Hughes, Tracey; Coelho, Helen; Cooper, Chris; Frayling, Ian; Hyde, Chris (September 2014). "A systematic review and economic evaluation of diagnostic strategies for Lynch syndrome". Health Technology Assessment. 18 (58): 1–406. doi:10.3310/hta18580. ISSN 1366-5278. PMC 4781313. PMID 25244061.
- ^ a b c Snowsill, Tristan; Coelho, Helen; Huxley, Nicola; Jones-Hughes, Tracey; Briscoe, Simon; Frayling, Ian M.; Hyde, Chris (September 2017). "Molecular testing for Lynch syndrome in people with colorectal cancer: systematic reviews and economic evaluation". Health Technology Assessment (Winchester, England). 21 (51): 1–238. doi:10.3310/hta21510. ISSN 2046-4924. PMC 5611555. PMID 28895526.
- ^ a b c Evrard, Camille; Tachon, Gaëlle; Randrian, Violaine; Karayan-Tapon, Lucie; Tougeron, David (2019-10-15). "Microsatellite Instability: Diagnosis, Heterogeneity, Discordance, and Clinical Impact in Colorectal Cancer". Cancers. 11 (10). doi:10.3390/cancers11101567. ISSN 2072-6694. PMC 6826728. PMID 31618962.
- ^ Hereditary Colorectal Cancer > Background. From Medscape. By Juan Carlos Munoz and Louis R Lambiase. Updated: Oct 31, 2011
- ^ Burn J, Bishop DT, Mecklin JP, Macrae F, Möslein G, Olschwang S, et al. (December 2008). "Effect of aspirin or resistant starch on colorectal neoplasia in the Lynch syndrome". The New England Journal of Medicine. 359 (24): 2567–78. doi:10.1056/NEJMoa0801297. hdl:10044/1/19614. PMID 19073976.
- ^ "Aspirin Confers Long-Term Protective Effect in Lynch Syndrome Patients". Retrieved 7 November 2009.
- ^ Vasen HF, Watson P, Mecklin JP, Lynch HT (June 1999). "New clinical criteria for hereditary nonpolyposis colorectal cancer (HNPCC, Lynch syndrome) proposed by the International Collaborative group on HNPCC". Gastroenterology. 116 (6): 1453–6. doi:10.1016/S0016-5085(99)70510-X. PMID 10348829.
- ^ a b c d e Vindigni, Stephen M.; Kaz, Andrew M. (2016). "Universal Screening of Colorectal Cancers for Lynch Syndrome: Challenges and Opportunities". Digestive Diseases and Sciences. 61 (4): 969–976. doi:10.1007/s10620-015-3964-6. ISSN 0163-2116.
- ^ a b c d Bui, Quan M.; Lin, David; Ho, Wendy (February 2017). "Approach to Lynch Syndrome for the Gastroenterologist". Digestive Diseases and Sciences. 62 (2): 299–304. doi:10.1007/s10620-016-4346-4. ISSN 0163-2116.
- ^ Boland CR, Koi M, Chang DK, Carethers JM (2007). "The biochemical basis of microsatellite instability and abnormal immunohistochemistry and clinical behavior in Lynch syndrome: from bench to bedside". Familial Cancer. 7 (1): 41–52. doi:10.1007/s10689-007-9145-9. PMC 2847875. PMID 17636426.
- ^ Le DT, Uram JN, Wang H, Bartlett BR, Kemberling H, Eyring AD, et al. (June 2015). "PD-1 Blockade in Tumors with Mismatch-Repair Deficiency". The New England Journal of Medicine. 372 (26): 2509–20. doi:10.1056/NEJMoa1500596. PMC 4481136. PMID 26028255.
- ^ Cancer Information, Research, and Treatment for all Types of Cancer | OncoLink Archived 2011-07-22 at the Wayback Machine
- ^ Lynch HT, Shaw MW, Magnuson CW, Larsen AL, Krush AJ (February 1966). "Hereditary factors in cancer. Study of two large midwestern kindreds". Archives of Internal Medicine. 117 (2): 206–12. doi:10.1001/archinte.117.2.206. PMID 5901552.
- ^ Bellizzi AM, Frankel WL (November 2009). "Colorectal cancer due to deficiency in DNA mismatch repair function: a review". Advances in Anatomic Pathology. 16 (6): 405–17. doi:10.1097/PAP.0b013e3181bb6bdc. PMID 19851131.
- ^ Lindor NM (October 2009). "Familial colorectal cancer type X: the other half of hereditary nonpolyposis colon cancer syndrome". Surgical Oncology Clinics of North America. 18 (4): 637–45. doi:10.1016/j.soc.2009.07.003. PMC 3454516. PMID 19793571.
- ^ Lindor NM, Rabe K, Petersen GM, Haile R, Casey G, Baron J, et al. (April 2005). "Lower cancer incidence in Amsterdam-I criteria families without mismatch repair deficiency: familial colorectal cancer type X". JAMA. 293 (16): 1979–85. doi:10.1001/jama.293.16.1979. PMC 2933042. PMID 15855431.
- ^ Scott RJ, McPhillips M, Meldrum CJ, Fitzgerald PE, Adams K, Spigelman AD, et al. (January 2001). "Hereditary nonpolyposis colorectal cancer in 95 families: differences and similarities between mutation-positive and mutation-negative kindreds". American Journal of Human Genetics. 68 (1): 118–127. doi:10.1086/316942. PMC 1234904. PMID 11112663.
- ^ Gologan A, Krasinskas A, Hunt J, Thull DL, Farkas L, Sepulveda AR (November 2005). "Performance of the revised Bethesda guidelines for identification of colorectal carcinomas with a high level of microsatellite instability". Archives of Pathology & Laboratory Medicine. 129 (11): 1390–7. doi:10.1043/1543-2165(2005)129[1390:POTRBG]2.0.CO;2 (inactive 2019-11-11). PMID 16253017.
- ^ Umar A, Boland CR, Terdiman JP, Syngal S, de la Chapelle A, Rüschoff J, et al. (February 2004). "Revised Bethesda Guidelines for hereditary nonpolyposis colorectal cancer (Lynch syndrome) and microsatellite instability". Journal of the National Cancer Institute. 96 (4): 261–8. doi:10.1093/jnci/djh034. PMC 2933058. PMID 14970275.
- ^ Lipton LR, Johnson V, Cummings C, Fisher S, Risby P, Eftekhar Sadat AT, et al. (December 2004). "Refining the Amsterdam Criteria and Bethesda Guidelines: testing algorithms for the prediction of mismatch repair mutation status in the familial cancer clinic". Journal of Clinical Oncology. 22 (24): 4934–43. doi:10.1200/JCO.2004.11.084. PMID 15611508.
- ^ "Lynch Syndrome UK". Retrieved 31 March 2018.
- ^ "Bowel Cancer UK: Lynch Syndrome". Retrieved 31 March 2018.
- ^ "CDC: March 22nd is National Lynch Syndrome Awareness Day!". 2018-03-20. Retrieved 31 March 2018.
External links[edit]
| Classification | |
|---|---|
| External resources |
No comments:
Post a Comment